ROLE OF PHYSIOTHRAPY IN AMPUTEE REHABILITATION
Raynaud’s syndrome
Raynaud’s phenomenon is a vasospastic disorder that affects the hands triggered by cold or emotional stress resulting in symptoms of pain, pallor progressing to cyanosis, and coolness of the distal extremities. These changes are thought to be due to intimal layer hypertrophy and inflammation; collagen disposition and fibrosis resulting in vessel lumen occlusion. These vascular alterations have been described in the digital arteries, superficial palmar arch and ulnar artery. Angiographic studies have demonstrated little or no collateral circulation distal to the fibrotic vessels. Radiographic findings in the hands may include soft tissue calcifications when the patient has Raynaud’s as part of CREST syndrome, atrophy of the finger tips, acroosteolysis and intercarpal joint space narrowing. The differential diagnosis for acroosteolysis includes: psoriasis, injury (frostbite or thermal burns), neuropathy (diabetes, leprosy, myelomeningocele), collagen vascular disease, hyperparathyroidism, polyvinyl chloride (PVC) exposure, snake/scorpion venom and familial forms (Hadju-Cheney syndrome).
role of family in health and disease
The importance of the family to family physicians is inherent in the paradigm of family medicine. Family medicine does not separate disease from person or person from environment. It recognizes the strong connection between health and disease, and personality, way of life, physical environment, and human relationships. It understands the strong influence that human relationships have on the outcome of illness and recognizes the family as the crucible of the development of the person. Clinicians can be minimally involved with a patient’s family; they may provide the family with information and advice; they may provide emotional support to help family members deal with the feelings aroused by having a family member with an illness; or they can carry out a systematic assessment of family function and plan an intervention designed to help a family deal with its problems. Cultural norms, differences in the form and function of “family,” and an understanding of the family life cycle, together with an understanding of individual development, must be taken into consideration by the practitioner.
Society, culture & health
Bringing and building social science theory to understand the social and cultural determinants of health, how society produces health and the lived experience.
The Society, Culture and Health theme contributes new thinking using social science theory to the social and cultural determinants of health. We seek to understand how health is experienced and produced within an ecological public health framework. Much of our research incorporates a focus on health inequalities and questions of health equity.
Our members – who are drawn from sociology, anthropology, epidemiology, economics and psychology – employ novel combinations of qualitative and quantitative methods as part of their own research projects as well as contributing to cross-disciplinary approaches to research within RSPH.
Our research in health, culture and society encompasses many aspects of the social and behavioural sciences in medicine. We are interested in how various psychological and sociological concepts are applied in practice and contribute to our understanding of health, disease and the care they require.
We have a wide range of methodological expertise, including qualitative and quantitative approaches, and specialise in ethnographic research as well as undertaking behavioural and neuroscientific studies.
Our specific interests include:
- Mental health and wellbeing
- Healthcare work practices and cultures
- Health and social inequalities
- Experiences of healthcare
- Psychosocial development
Our work is often collaborative and we engage with a wide range of NHS and third sector organisations. We work with patients, families and carers, healthcare practitioners, and policy makers. Our focus is on improving the practices of care as well as furthering insights across health and medicine.
Breast cyst
REQUEST AN APPOINTMENT OR BOOK A CONSULANT – Sargam.dange.18@gmail.com
Breast cysts are fluid-filled sacs that are among the most common breast lumps a woman may have. They may also be a cause of other breast symptoms—from pain to, potentially, nipple discharge.
Many women develop noncancerous changes in their breast tissue. It’s one of the conditions known as fibrocystic breast disease, which includes fluid-filled cysts. A cyst may show up in one or both breasts at the same time and in different parts of the breast. Some cysts are so small that patients don’t feel a lump.
For many patients, breast cysts don’t have symptoms: Only about 7 percent of women have a breast cyst that may be felt with the hand.
Simple fluid-filled cysts form from fluid buildup in the breast glands. Microcysts are tiny and may only be spotted under a microscope. Macrocysts, on the other hand, may span from 1 to 2 inches.
Then there are complex cysts, which are either solid or filled with fluid and solids. A complex breast cyst may require a biopsy and drainage to check the cells, a procedure designed to determine whether the cyst is cancerous. On rare occasions, complex cysts are cancerous or increase the risk of breast cancer later.
Symptoms
Breast cysts may be found in one or both breasts. Signs and symptoms of a breast cyst include:
- A smooth, easily movable round or oval lump that may have smooth edges — which typically, though not always, indicates it’s benign
- Nipple discharge that may be clear, yellow, straw colored or dark brown
- Breast pain or tenderness in the area of the breast lump
- An increase in breast lump size and breast tenderness just before your period
- A decrease in breast lump size and resolution of other symptoms after your period
Having breast cysts doesn’t increase your risk of breast cancer. But having cysts may make it harder to find new breast lumps or other changes that might need evaluation by your doctor. Your breasts may feel lumpy and painful when you’re menstruating, so it’s important to be familiar with how your breasts feel throughout your menstrual cycle so that you’ll know if something changes.
When to see a doctor
Normal breast tissue often feels lumpy or nodular. But if you feel a new breast lump that doesn’t go away, gets bigger or persists after one or two menstrual cycles, see your doctor right away. Also see your doctor if you have new skin changes on one or both of your breasts.
Causes
Each of your breasts contains lobes of glandular tissue, arranged like petals of a daisy. The lobes are divided into smaller lobules that produce milk during pregnancy and breast-feeding. The supporting tissue that gives the breast its shape is made up of fatty tissue and fibrous connective tissue. Breast cysts develop as a result of fluid accumulation inside the glands in the breasts.
Breast cysts may be defined by their size:
- Microcysts may be seen during imaging tests, such as mammography or ultrasound, but are too small to feel.
- Macrocysts are large enough to be felt and can grow to about 1 to 2 inches (2.5 to 5 centimeters) in diameter.
Experts don’t know exactly what causes breast cysts. They may develop as a result of hormonal changes from monthly menstruation.
REQUEST AN APPOINTMENT OR BOOK A CONSULANT – Sargam.dange.18@gmail.com
Diagnosis
Diagnosis of a breast cyst usually includes a breast exam; imaging tests, such as a breast ultrasound or mammogram; and possibly fine-needle aspiration or a breast biopsy.
Breast exam
After discussing your symptoms and health history, your doctor will physically examine the breast lump and check for any other breast abnormalities. Because your doctor can’t tell from a clinical breast exam alone whether a breast lump is a cyst, you’ll need another test. This is usually either an imaging test or fine-needle aspiration.
Imaging tests
Needed tests may include:
- Mammography. Large cysts and clusters of small cysts can usually be seen with mammography. But microcysts can be difficult or impossible to see on a mammogram.
- Breast ultrasound. This test can help your doctor determine whether a breast lump is fluid filled or solid. A fluid-filled area usually indicates a breast cyst. A solid-appearing mass most likely is a noncancerous lump, such as a fibroadenoma, but solid lumps also could be breast cancer.
Your doctor may recommend a biopsy to further evaluate a mass that appears solid. If your doctor can easily feel a breast lump, he or she may skip imaging tests and perform fine-needle aspiration to drain the fluid and collapse the cyst.
Fine-needle aspiration
During a fine-needle aspiration, your doctor inserts a thin needle into the breast lump and attempts to withdraw (aspirate) fluid. Often, fine-needle aspiration is done using ultrasound to guide accurate placement of the needle. If fluid comes out and the breast lump goes away, your doctor can make a breast cyst diagnosis immediately.
- If the fluid is not bloody and has a straw-colored appearance and the breast lump disappears, you need no further testing or treatment.
- If the fluid appears bloody or the breast lump doesn’t disappear, your doctor may send a sample of the fluid for lab testing and refer you to a breast surgeon or to a radiologist — a doctor trained to perform imaging exams and procedures — for follow-up.
- If no fluid is withdrawn, your doctor will likely recommend an imaging test, such as a diagnostic mammogram or ultrasound. The lack of fluid or a breast lump that doesn’t disappear after aspiration suggests that the breast lump — or at least a portion of it — is solid. A sample of the tissue may be collected to check for cancer.
Treatment
No treatment is necessary for simple breast cysts — those that are fluid filled and don’t cause any symptoms — that are confirmed on breast ultrasound or after a fine-needle aspiration. Many cysts will disappear with no treatment. If a cyst persists, feels firmer or you notice skin changes on the skin over the cyst, follow up with your doctor.
Fine-needle aspiration
Fine-needle aspiration may be used to diagnose and treat a breast cyst if all the fluid can be removed from the cyst during the procedure, and then your breast lump disappears and your symptoms resolve.
For some breast cysts, however, you may need to have fluid drained more than once. Recurrent or new cysts are common. If a breast cyst persists through two to three menstrual cycles and grows larger, see your doctor for further evaluation.
Hormone use
Using birth control pills (oral contraceptives) to regulate your menstrual cycles may help reduce the recurrence of breast cysts. But because of possible significant side effects, birth control pills or other hormone therapy, such as tamoxifen, is usually recommended only for women with severe symptoms. Discontinuing hormone therapy after menopause may also help prevent breast cysts.
Surgery
Surgery to remove a breast cyst is necessary only in unusual circumstances. Surgery may be considered if an uncomfortable breast cyst recurs month after month or if a breast cyst contains blood-tinged fluid or shows other worrisome signs.
REQUEST AN APPOINTMENT OR BOOK A CONSULANT – Sargam.dange.18@gmail.com
Fibroadenoma
REQUEST AN APPOINTMENT OR BOOK A CONSULANT – Sargam.dange.18@gmail.com
Breast fibroadenomas are the most common type of noncancerous (benign) breast tumor. They are often described as round, moveable, painless breast lumps that feel smooth and rubbery. They can be felt during your monthly breast self-exam and will show up on mammograms and ultrasounds.
Fibroadenomas usually occur in premenopausal women. They may grow during pregnancy, breastfeeding, or estrogen therapy.
Although fibroadenomas have a typical feel on physical examination and appearance on breast ultrasound, the only way to ensure a breast lump is a fibroadenoma is through a biopsy. Proven fibroadenomas may not need treatment unless they are large, fast-growing, or cause bothersome symptoms.
A fibroadenoma is a solid breast lump. This breast lump is not cancer. A fibroadenoma happens most often between ages 15 and 35. But it can be found at any age in anyone who has periods.
A fibroadenoma often causes no pain. It can feel firm, smooth and rubbery. It has a round shape. It might feel like a pea in the breast. Or it may feel flat like a coin. When touched, it moves easily within the breast tissue.
Fibroadenomas are common breast lumps. If you have a fibroadenoma, your health care provider may tell you to watch for changes in its size or feel. You may need a biopsy to check the lump or surgery to remove it. Many fibroadenomas need no further treatment.
Symptoms
A fibroadenoma is a solid breast lump that often causes no pain. It is:
- Round with distinct, smooth borders
- Easily moved
- Firm or rubbery
A fibroadenoma often grows slowly. The average size is about 1 inch (2.5 centimeters). A fibroadenoma can get bigger over time. It may be tender or cause soreness a few days before your period. A large fibroadenoma may hurt when you touch it. But most often, this type of breast lump causes no pain.
You can have a single fibroadenoma or more than one fibroadenoma. They can occur in one or both breasts.
Some fibroadenomas shrink over time. Most fibroadenomas in adolescents shrink over many months to a few years. They then disappear. Fibroadenomas may also change shape over time.
Fibroadenomas may get bigger during pregnancy. They might shrink after menopause.
When to see a doctor
Healthy breast tissue often feels lumpy. Make an appointment with your health care provider if you:
- Find a new breast lump
- Notice other changes in your breasts
- Find that a breast lump you had checked in the past has grown or changed in any way
REQUEST AN APPOINTMENT OR BOOK A CONSULANT – Sargam.dange.18@gmail.com
Causes
The cause of fibroadenomas is not known. They might be related to hormones that control your periods.
Less common types of fibroadenomas and related breast lumps may not act the same as typical fibroadenomas. These types of breast lumps include:
- Complex fibroadenomas. These are fibroadenomas that can get bigger over time. They can press on or displace nearby breast tissue.
- Giant fibroadenomas. Giant fibroadenomas grow quickly to larger than 2 inches (5 centimeters). They also can press on nearby breast tissue or push it out of place.
- Phyllodes tumors. Phyllodes tumors and fibroadenomas are made of similar tissues. But under a microscope, phyllodes tumors look different from fibroadenomas. Phyllodes tumors typically have features associated with growing faster. Most phyllodes tumors are benign. This means they are not cancer. But some phyllodes tumors may be cancer. Or they could become cancer. Phyllodes tumors often cause no pain.
Complications
Common fibroadenomas do not affect your risk of breast cancer. But your risk might go up a bit if you have a complex fibroadenoma or a phyllodes tumor.
Diagnosis
A fibroadenoma may first be discovered on physical examination or during a routine screening mammogram. On a mammogram, fibroadenomas appear as round or oval smooth-edged masses. The outline will be clearly defined, not blurry, and will not be invading the adjacent spaces. Sometimes they are accompanied by coarse calcifications (calcium deposits). Fibroadenomas can look like cysts or a well-contained tumor.
If you notice a lump during an exam or if an abnormality is seen on mammography, a breast ultrasound is usually the next step. This is especially true if you have dense breast tissue, which can make a lump more difficult to view.
On ultrasound, a fibroadenoma will be easier to distinguish from other tissue because of the way it responds to sound waves. It will appear as a dark area with a definite outline. It will look homogeneous (looks the same throughout), round or oval, and may have smooth-edged bumps.
Your doctor may also order digital breast tomosynthesis (DBT), a specialized form of mammography that creates 3D images of the breast, and allows a more detailed evaluation when compared to a regular mammogram.
Biopsy
While imaging tests may suggest a fibroadenoma, the conclusive diagnostic test is usually a breast biopsy, a procedure to remove a sample of tissue for examination in a lab.
Different types of biopsy procedures include fine-needle aspiration or core-needle biopsy, both of which use needles to extract tissue, and open biopsy, a surgical procedure in which a cut is made in the skin to extract sample tissue. Which type your healthcare provider chooses will depend on the characteristics of the lump, its location, and other factors. In women at increased risk for breast cancer, your healthcare provider may strongly recommend surgical removal.
As with any biopsy, breast biopsies carry a risk of a false-negative result that is, the test detects no cancer when cancer is actually present). This is because a breast biopsy may only sample one part of a lump and could miss the cancerous portion. For this reason, you should continue routine breast cancer screening even if you have had a benign biopsy in the past.
Fibroadenoma Treatment
It’s important to distinguish between the two types of fibroadenomas when choosing the best treatment options because of the difference in associated breast cancer risk.
Fibroadenomas are classified as either:
- Simple: Most fibroadenomas are the simple type; they are more common in younger people. There’s usually just one mass in your breast, with a definite border and very uniform cells. A simple fibroadenoma does not raise your risk for breast cancer.
- Complex: Complex fibroadenomas are less common but become more common as people age. While they may have a definite border, it’s what is inside this kind of fibroadenoma that makes it different. Under a microscope, a complex fibroadenoma will not look organized and uniform like a simple one. There is often evidence of rapidly dividing cells (hyperplasia) that may have an abnormal appearance (atypia). Having a complex fibroadenoma can raise your risk of developing breast cancer,
Aside from fibroadenoma type, other factors may influence treatment choice, such as:
- Symptoms, especially discomfort and pain
- Emotional state, such as undue worry about it being cancer
Be open and honest with your healthcare provider about what you’re experiencing so your concerns can be considered when weighing treatment options.
In considering all of this, your healthcare provider will recommend one of the following fibroadenoma treatment options.
Watch and Wait
Since fibroadenomas are not always troublesome and sometimes shrink on their own, just keeping an eye on their progress is the least invasive way to handle them.
Laser Ablation
In your surgeon’s office, an ultrasound-guided laser device is used to destroy the fibroadenoma, leaving behind only a tiny scar, no sutures, and no change in breast shape. You don’t need general anesthesia, and it’s usually an outpatient procedure, which means no hospital stay.
Cryoablation
Cryoablation is a fast, efficient way to freeze a fibroadenoma. In one office visit, the healthcare provider simply freezes the lump so that healthy tissue can take over. This procedure takes less than 30 minutes and results in a tiny scar.
Radiofrequency Ablation (RFA)
This is a way to remove fibroadenomas without resorting to a lumpectomy. Using local anesthesia and ultrasound guidance, a 6- to 8-millimeter (about 1/4 inch to nearly 1/3 inch) cut is made above the fibroadenoma. Through this cut, a surgical wand is inserted and then tipped by a knife that is heated by radiofrequency current. This helps cut through the breast tissue without causing much bleeding. Once it reaches the target, small wires and robotic arms capture the fibroadenoma and extract it.
Vacuum-Assisted Excision
Breast biopsy systems can now be used as a mostly noninvasive way to remove small fibroadenomas. In less than an hour, and under local anesthesia, a 6-millimeter (1/4 inch) cut is made over the fibroadenoma. Then, with ultrasound guidance, a probe is threaded into the lump, which vacuums out sections of the tissue. Recovery is quick and your scar will be quite small.
High-Frequency Focused Ultrasound (HFU)
This is a relatively new treatment that has been used for fibroadenomas and, sometimes, even for breast cancer. HFU appears to cause the selective destruction of deep tissues without damaging surrounding healthy tissue.
Lumpectomy
Surgical removal can be done if you’re worried about a fibroadenoma. Depending on the relative size of the lump and your breast, a lumpectomy may cause a change in your breast’s size or shape. New fibroadenomas may grow in the area of the first lump, so you should know that surgery is not a guarantee that you’ll never have another fibroadenoma. On the other hand, your fibroadenoma can be carefully examined by a pathologist to make sure your diagnosis is correct.
For pain that may be due to a fibroadenoma, over-the-counter pain medications and applied heat are often used.
Complementary and Alternative Medicine (CAM) Concerns
Certain herbal supplements and diets have been touted as effective treatments for fibroadenomas or their symptoms, but few controlled studies have looked into these remedies. Adopting a healthy lifestyle, including regular exercise and eating lots of fruits and vegetables, is always good advice and may help relieve fibroadenoma symptoms. But remember that these interventions shouldn’t replace proper testing.
REQUEST AN APPOINTMENT OR BOOK A CONSULANT – Sargam.dange.18@gmail.com
Mastalgia
REQUEST AN APPOINTMENT OR BOOK A CONSULANT – Sargam.dange.18@gmail.com
Breast pain (mastalgia) can be described as tenderness, throbbing, sharp, stabbing, burning pain or tightness in the breast tissue. The pain may be constant or it may occur only occasionally, and it can occur in men, women and transgender people.
Breast pain can range from mild to severe. It may occur:
- Just a few days a month, in the two to three days leading up to a menstrual period. This normal, mild-to-moderate pain affects both breasts.
- A week or longer each month, starting before a period and sometimes continuing through the menstrual cycle. The pain may be moderate or severe, and affects both breasts.
- Throughout the month, not related to a menstrual cycle.
In men, breast pain is most commonly caused by a condition called “gynecomastia” (guy-nuh-koh-MAS-tee-uh). This refers to an increase in the amount of breast gland tissue that’s caused by an imbalance of the hormones estrogen and testosterone. Gynecomastia can affect one or both breasts, sometimes unevenly.
In transgender women, hormone therapy may cause breast pain. In transgender men, breast pain may be caused by the minimal amount of breast tissue that may remain after a mastectomy.
Most times, breast pain signals a noncancerous (benign) breast condition and rarely indicates breast cancer. Unexplained breast pain that doesn’t go away after one or two menstrual cycles, or that persists after menopause, or breast pain that doesn’t seem to be related to hormone changes needs to be evaluated.

Causes
Mastalgia can be broken down into two separate categories: cyclic and noncyclic. The causes vary, depending on the kind of mastalgia it is.
Cyclic Mastalgia
Cyclic mastalgia is breast pain that’s related to the hormonal variations associated with the menstrual cycle, which affect how your breasts feel over the course of a month.
The pain is often described as a dull, heavy ache, not focused on any specific spot. It affects both breasts and the armpit areas.
Cyclic mastalgia is typically at its worst shortly before the cycle begins, decreasing on the first day of your period and then going away over the next few days. If hormones are the cause, the symptoms should decrease at certain times during your monthly cycle.
Noncyclic Mastalgia
Noncyclic mastalgia is breast pain that doesn’t vary with the menstrual cycle or with hormonal changes. In postmenopausal females, most breast pain is noncyclic, but you can have it before menopause as well.
The pain may be described as sharp or burning and is often felt only in one breast and one particular area of that breast. It’s also known as “trigger zone” breast pain because you can point to where it hurts. It’s most common between the ages of 30 and 50.1
Noncyclical breast pain is often related to:
- An injury
- Surgery
- Infections
- Breast fibroadenoma, or a breast cyst
- Inflammatory breast cancer
Large breasts (either from obesity or genetics) may also be a source of noncyclic mastalgia. They can be especially painful if a supportive bra is not worn. This is due to the stretching of Cooper’s ligaments, which are bands of connective tissue that support and shape breast tissue.
Since this type of pain is linked to menstruation, premenopausal females are most likely to experience it. Cyclical breast pain can also be associated with oral contraceptive pills and HRT.
Fibrocystic breast changes, which can cause breast pain, swelling, or thick areas, involve the lobes, ducts, and connective tissue.
Noncyclic Mastalgia
Noncyclic mastalgia is breast pain that doesn’t vary with the menstrual cycle or with hormonal changes.In postmenopausal females, most breast pain is noncyclic, but you can have it before menopause as well.
The pain may be described as sharp or burning and is often felt only in one breast and one particular area of that breast. It’s also known as “trigger zone” breast pain because you can point to where it hurts. It’s most common between the ages of 30 and 50.1
Noncyclical breast pain is often related to:
- An injury
- Surgery
- Infections
- Breast fibroadenoma, or a breast cyst
- Inflammatory breast cancer
Large breasts (either from obesity or genetics) may also be a source of noncyclic mastalgia. They can be especially painful if a supportive bra is not worn. This is due to the stretching of Cooper’s ligaments, which are bands of connective tissue that support and shape breast tissue.
Extramammary breast pain
The term “extramammary” means “outside the breast.” Extramammary breast pain feels like it starts in the breast tissue, but its source is actually outside the breast area. Pulling a muscle in the chest, for example, can cause pain in the chest wall or rib cage that spreads (radiates) to the breast. Arthritis that involves the cartilage in the chest, also known as costochondritis, can also cause pain.
When to see a doctor
REQUEST AN APPOINTMENT OR BOOK A CONSULANT – Sargam.dange.18@gmail.com
Make an appointment with your doctor if breast pain:
- Continues daily for more than a couple of weeks
- Occurs in one specific area of your breast
- Seems to be getting worse over time
- Interferes with daily activities
- Awakens you from sleep
Breast cancer risk is very low in people whose main symptom is breast pain, but if your doctor recommends an evaluation, it’s important to follow through.
Diagnosis
The diagnosis of mastalgia is most often made based on symptoms and a physical breast exam, though imaging studies may be done to further evaluate abnormalities noted during a physical exam.
The chance of mastalgia being a symptom of breast cancer is quite low, but it’s important to screen women who are at risk.
Breast cancer is often painless, but breast pain can be a symptom of the disease. If you do have breast pain, call your doctor for an appointment right away.
Treatment
The best treatment for your breast pain depends on what is causing it.
For both cyclic and noncyclic pain, reassurance and ruling out breast cancer is often a relief. If treatment is needed, there are effective treatment options.
Home Remedies
Many home remedies have been tried to decrease cyclic and noncyclic pain, sometimes with good results.
They include:
- Wearing a well-fitting bra: This can help contain painful breasts and keep them from being pulled uncomfortably.
- Practicing stress relief: Increased stress can affect hormone levels and lead to more discomfort.
- Exercising: Physical activity decreases estrogen, but it’s difficult to tell from studies if it really decreases mastalgia.
- Reducing caffeine and eating a low-fat diet: Studies are mixed on how well this works, but it may help some women.
Keeping a journal can also be helpful, especially if you’re trying to see a pattern in your symptoms, which is the best way to determine the kind of breast pain you have.
Medications
Easing pain with Tylenol (acetaminophen) or nonsteroidal anti-inflammatory drugs (NSAIDs) like Advil (ibuprofen) is another option.
If these first-line interventions don’t help, your healthcare provider may suggest prescription medications like Nolvadex (tamoxifen) and Danocrine (danazol). All of these drugs have side effects of their own.
Studies appeared to show the greatest benefit with tamoxifen, but Danocrine is the only medication approved by the Food and Drug Administration (FDA) for treating mastalgia at this time.
REQUEST AN APPOINTMENT OR BOOK A CONSULANT – Sargam.dange.18@gmail.com
Raynaud’s syndrome
REQUEST AN APPOINTMENT OR BOOK A CONSULANT – Sargam.dange.18@gmail.com
Raynaud’s disease causes some areas of the body — such as fingers and toes — to feel numb and cold in response to cold temperatures or stress. In Raynaud’s disease, smaller arteries that supply blood to the skin narrow. This limits blood flow to affected areas, which is called vasospasm.
Other names for this condition are:
- Raynaud’s phenomenon.
- Raynaud syndrome.
Raynaud’s phenomenon is a vasospastic disorder that affects the hands triggered by cold or emotional stress resulting in symptoms of pain, pallor progressing to cyanosis, and coolness of the distal extremities. These changes are thought to be due to intimal layer hypertrophy and inflammation; collagen disposition and fibrosis resulting in vessel lumen occlusion. These vascular alterations have been described in the digital arteries, superficial palmar arch and ulnar artery. Angiographic studies have demonstrated little or no collateral circulation distal to the fibrotic vessels. Radiographic findings in the hands may include soft tissue calcifications when the patient has Raynaud’s as part of CREST syndrome, atrophy of the finger tips, acroosteolysis and intercarpal joint space narrowing. The differential diagnosis for acroosteolysis includes: psoriasis, injury (frostbite or thermal burns), neuropathy (diabetes, leprosy, myelomeningocele), collagen vascular disease, hyperparathyroidism, polyvinyl chloride (PVC) exposure, snake/scorpion venom and familial forms (Hadju-Cheney syndrome).
Symptoms
Symptoms of Raynaud’s disease include:
- Cold fingers or toes.
- Areas of skin that turn white then blue. Depending on your skin color, these color changes may be harder or easier to see.
- Numb, prickly feeling or stinging pain upon warming or stress relief.
During an attack of Raynaud’s, affected areas of the skin usually first turn pale. Next, they often change color and feel cold and numb. When the skin warms and blood flow improves, the affected areas may change color again, throb, tingle or swell.
Raynaud’s most commonly affects fingers and toes. But it also can affect other areas of the body, such as nose, lips, ears and even nipples. After warming up, the return of blood flow to the area can take 15 minutes.
When to see a doctor
See your health care provider right away if you have a history of severe Raynaud’s and get a sore or infection in one of your affected fingers or toes.
Causes
Experts don’t fully understand the cause of Raynaud’s attacks. But blood vessels in the hands and feet appear to react too strongly to cold temperatures or stress.
With Raynaud’s, arteries to the fingers and toes narrow when exposed to cold or stress. The narrowed arteries limit blood flow. Over time, these small arteries can thicken slightly and limit blood flow even more.
Cold temperatures are the most likely cause of an attack. Examples are putting hands in cold water, taking something from a freezer or being in cold air. For some people, emotional stress can trigger an episode.
REQUEST AN APPOINTMENT OR BOOK A CONSULANT – Sargam.dange.18@gmail.com
Primary vs. secondary Raynaud’s
There are two main types of the condition.
- Primary Raynaud’s. Also called Raynaud’s disease, this most common form isn’t the result of another medical condition. It can be so mild that many people with primary Raynaud’s don’t seek treatment. And it can go away on its own.
- Secondary Raynaud’s. Also called Raynaud’s phenomenon, this form develops because of another health condition. Although secondary Raynaud’s is less common than the primary form, it tends to be more serious.Symptoms of secondary Raynaud’s usually appear around age 40. That’s later than symptoms appear for primary Raynaud’s.
Causes of secondary Raynaud’s include:
- Connective tissue diseases. Most people who have a rare disease that leads to hardening and scarring of the skin, known as scleroderma, have Raynaud’s. Other diseases that increase the risk of Raynaud’s include lupus, rheumatoid arthritis and Sjogren’s syndrome.
- Diseases of the arteries. These include a buildup of fatty deposits in blood vessels that feed the heart and a disorder in which the blood vessels of the hands and feet become inflamed. A type of high blood pressure that affects the arteries of the lungs also may cause secondary Raynaud’s.
- Carpal tunnel syndrome. This condition involves pressure on a major nerve to the hand. The pressure causes numbness and pain in the hand that can make the hand react more to cold temperatures.
- Repeated actions or vibration. Typing, playing piano or doing movements like that for long periods can cause overuse injuries. So can using vibrating tools, such as jackhammers.
- Smoking. Smoking narrows blood vessels.
- Injuries to the hands or feet. Examples include a wrist fracture, surgery or frostbite.
- Certain medicines. These include beta blockers for high blood pressure, some migraine medicines, attention-deficit/hyperactivity disorder medicines, certain cancer medicines and some cold medicines.
Risk factors
Risk factors for primary Raynaud’s include:
- Sex. The condition affects more women than men.
- Age. Although anyone can develop the condition, primary Raynaud’s often begins between the ages of 15 and 30.
- Climate. The illness also is more common in people who live in colder climates.
- Family history. Having a parent, sibling or child with the disease appears to increase the risk of primary Raynaud’s.
Risk factors for secondary Raynaud’s include:
- Certain diseases. These include conditions such as scleroderma and lupus.
- Certain jobs. These include jobs that cause repeated trauma, such as using tools that vibrate.
- Certain substances. This includes smoking, taking medicines that affect the blood vessels and being around certain chemicals, such as vinyl chloride.
Complications
If secondary Raynaud’s is severe, reduced blood flow to fingers or toes could cause tissue damage. But that’s rare.
A completely blocked artery can lead to skin sores or dead tissue. This can be difficult to treat. Rarely, very bad untreated instances might require removing the affected part of the body.
Prevention
To help prevent Raynaud’s attacks:
- Bundle up outdoors. When it’s cold, wear a hat, scarf, socks and boots, and two sets of mittens or gloves. Thermal underwear might help. A coat with cuffs that close around mittens or gloves helps protect the hands from cold air.Wear earmuffs and a face mask if the tip of your nose and your earlobes get too cold.
- Warm your car. Run your car heater for a few minutes before driving in cold weather.
- Take care indoors. Wear socks. To take food out of the refrigerator or freezer, wear gloves, mittens or oven mitts. Some people find it helpful to wear mittens and socks to bed during winter.Because air conditioning can cause attacks, set your air conditioner to a warmer temperature. Use drinking glasses that keep hands from feeling cold.
REQUEST AN APPOINTMENT OR BOOK A CONSULANT – Sargam.dange.18@gmail.com
skin tumors
REQUEST AN APPOINTMENT OR BOOK A CONSULANT – Sargam.dange.18@gmail.com
Skin cancer — the abnormal growth of skin cells — most often develops on skin exposed to the sun. But this common form of cancer can also occur on areas of your skin not ordinarily exposed to sunlight.
There are three major types of skin cancer — basal cell carcinoma, squamous cell carcinoma and melanoma.
You can reduce your risk of skin cancer by limiting or avoiding exposure to ultraviolet (UV) radiation. Checking your skin for suspicious changes can help detect skin cancer at its earliest stages. Early detection of skin cancer gives you the greatest chance for successful skin cancer treatment.
Symptoms
Where skin cancer develops
 Basal cell carcinoma on white skinEnlarge image
Basal cell carcinoma on white skinEnlarge image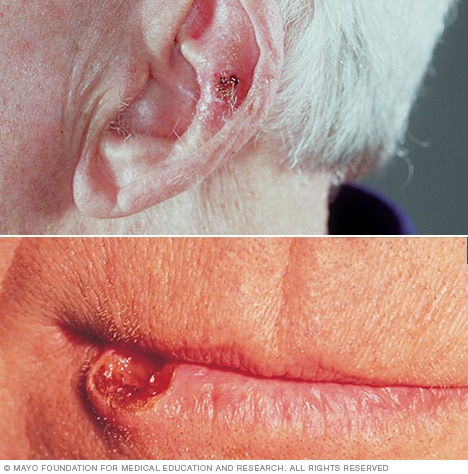 Squamous cell carcinoma of the skinEnlarge image
Squamous cell carcinoma of the skinEnlarge image MelanomaEnlarge image
MelanomaEnlarge image Merkel cell carcinomaEnlarge image
Merkel cell carcinomaEnlarge image
Skin cancer develops primarily on areas of sun-exposed skin, including the scalp, face, lips, ears, neck, chest, arms and hands, and on the legs in women. But it can also form on areas that rarely see the light of day — your palms, beneath your fingernails or toenails, and your genital area.
Skin cancer affects people of all skin tones, including those with darker complexions. When melanoma occurs in people with dark skin tones, it’s more likely to occur in areas not normally exposed to the sun, such as the palms of the hands and soles of the feet.
Basal cell carcinoma signs and symptoms
Basal cell carcinoma usually occurs in sun-exposed areas of your body, such as your neck or face.
Basal cell carcinoma may appear as:
- A pearly or waxy bump
- A flat, flesh-colored or brown scar-like lesion
- A bleeding or scabbing sore that heals and returns
Squamous cell carcinoma signs and symptoms
Most often, squamous cell carcinoma occurs on sun-exposed areas of your body, such as your face, ears and hands. People with darker skin are more likely to develop squamous cell carcinoma on areas that aren’t often exposed to the sun.
Squamous cell carcinoma may appear as:
- A firm, red nodule
- A flat lesion with a scaly, crusted surface
Melanoma signs and symptoms
Melanoma can develop anywhere on your body, in otherwise normal skin or in an existing mole that becomes cancerous. Melanoma most often appears on the face or the trunk of affected men. In women, this type of cancer most often develops on the lower legs. In both men and women, melanoma can occur on skin that hasn’t been exposed to the sun.
Melanoma can affect people of any skin tone. In people with darker skin tones, melanoma tends to occur on the palms or soles, or under the fingernails or toenails.
Melanoma signs include:
- A large brownish spot with darker speckles
- A mole that changes in color, size or feel or that bleeds
- A small lesion with an irregular border and portions that appear red, pink, white, blue or blue-black
- A painful lesion that itches or burns
- Dark lesions on your palms, soles, fingertips or toes, or on mucous membranes lining your mouth, nose, vagina or anus
Signs and symptoms of less common skin cancers
Other, less common types of skin cancer include:
- Kaposi sarcoma. This rare form of skin cancer develops in the skin’s blood vessels and causes red or purple patches on the skin or mucous membranes.Kaposi sarcoma mainly occurs in people with weakened immune systems, such as people with AIDS, and in people taking medications that suppress their natural immunity, such as people who’ve undergone organ transplants.Other people with an increased risk of Kaposi sarcoma include young men living in Africa or older men of Italian or Eastern European Jewish heritage.
- Merkel cell carcinoma. Merkel cell carcinoma causes firm, shiny nodules that occur on or just beneath the skin and in hair follicles. Merkel cell carcinoma is most often found on the head, neck and trunk.
- Sebaceous gland carcinoma. This uncommon and aggressive cancer originates in the oil glands in the skin. Sebaceous gland carcinomas — which usually appear as hard, painless nodules — can develop anywhere, but most occur on the eyelid, where they’re frequently mistaken for other eyelid problems.
When to see a doctor
Make an appointment with your doctor if you notice any changes to your skin that worry you. Not all skin changes are caused by skin cancer. Your doctor will investigate your skin changes to determine a cause.
REQUEST AN APPOINTMENT OR BOOK A CONSULANT – Sargam.dange.18@gmail.com
pathophysiology
Although the exact etiology of BCC is unknown, a well-established relationship exists between BCC and the pilosebaceous unit, as tumors are most often discovered on hair-bearing areas.
Many believe that BCCs arise from pluripotential cells in the basal layer of the epidermis or follicular structures. These cells form continuously during life and can form hair, sebaceous glands, and apocrine glands. Tumors usually arise from the epidermis and occasionally arise from the outer root sheath of a hair follicle, specifically from hair follicle stem cells residing just below the sebaceous gland duct in an area called the bulge.
Signaling pathways
The patched/hedgehog intracellular signaling pathway plays a role in both sporadic BCCs and nevoid BCC syndrome (Gorlin syndrome). This pathway influences differentiation of various tissues during fetal development. After embryogenesis, it continues to function in regulation of cell growth and differentiation. Loss of inhibition of this pathway is associated with human malignancy, including BCC.
The hedgehog gene encodes an extracellular protein that binds to a cell membrane receptor complex to start a cascade of cellular events leading to cell proliferation. Of the 3 known human homologues, sonic hedgehog (SHH) protein is the most relevant to BCC. Patched (PTCH) is a protein that is the ligand-binding component of the hedgehog receptor complex in the cell membrane. The other protein member of the receptor complex, smoothened (SMO), is responsible for transducing hedgehog signaling to downstream genes.
When SHH is present, it binds to PTCH, which then releases and activates SMO. SMO signaling is transduced to the nucleus via Gli. When SHH is absent, PTCH binds to and inhibits SMO. Mutations in the PTCH gene prevent it from binding to SMO, simulating the presence of SHH. The unbound SMO and downstream Gli are constitutively activated, thereby allowing hedgehog signaling to proceed unimpeded. The same pathway may also be activated via mutations in the SMO gene, which also allows unregulated signaling of tumor growth.
How these defects cause tumorigenesis is not fully understood, but most BCCs have abnormalities in either PTCH or SMO genes. Some even consider defects in the hedgehog pathway to be requirements for BCC development.
BCC most commonly develops on sun-exposed areas. Zhang et al reported that ultraviolet (UV)-specific nucleotide changes in PTCH, as well as the tumor suppressor gene TP53, are implicated in the development of early-onset BCC.
UV-induced mutations in the TP53 tumor suppressor gene, which resides on band 17p13.1, have been found in some cases of BCC. A germline single-nucleotide polymorphism (SNP) in the TP53 gene, rs78378222, has also been associated with susceptibility to BCC. In addition, frameshift mutations of the BAX gene (BCL2-associated X protein) have been found in sporadic cases of BCC. A reduction of bcl-2 proteins is observed in the aggressive, infiltrative type of BCC.
REQUEST AN APPOINTMENT OR BOOK A CONSULANT – Sargam.dange.18@gmail.com
Radiation and immunologic origins
Radiation has proven to be tumorigenic by two mechanisms. The first entails the initiations of prolonged cellular proliferation, thereby increasing the likelihood of transcription errors that can lead to cellular transformation. The second mechanism is direct damage of DNA replication, leading to cellular mutation that may activate proto-oncogenes or deactivate tumor suppressor genes.
Immunologically, the mechanism by which prolonged ultraviolet radiation exposure leads to the development of BCC includes suppression of the cutaneous immune system and immunologic unresponsiveness to cutaneous tumors. This local effect includes a decrease in Langerhans cells, dendritic epidermal T cells, and Thy1+ cells. Furthermore, systemic proliferation of suppressor T cells and the release of immunosuppressive factors (eg, tumor necrosis factor-alpha [TNF-alpha], interleukin 1 [IL-1], prostaglandin [PG], interleukin 10 [IL-10]) are believed to be pathogenic to the development of BCC.
DNA mismatch repair proteins
DNA mismatch repair (MMR) proteins are a group of proteins that physiologically stimulate G2 cell cycle checkpoint arrest and apoptosis. Failure of MMR proteins to detect induced DNA damage results in the survival of mutating cells. MMR protein levels have been found to be higher in nonmelanoma skin cancers than in normal skin, and there is also some evidence of MMR dysregulation.