The uterus (womb) is a muscular structure that’s held in place by pelvic muscles and ligaments. If these muscles or ligaments stretch or become weak, they’re no longer able to support the uterus, causing prolapse.
Uterine prolapse occurs when the uterus sags or slips from its normal position and into the vagina (birth canal).
Uterine prolapse may be incomplete or complete. An incomplete prolapse occurs when the uterus is only partly sagging into the vagina. A complete prolapse occurs when the uterus falls so far down that some tissue protrudes outside of the vagina.
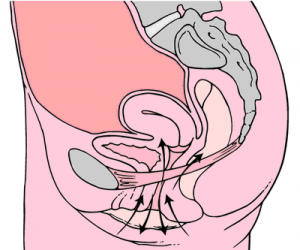
Uterine prolapse occurs when pelvic floor muscles and ligaments stretch and weaken and no longer provide enough support for the uterus. As a result, the uterus slips down into or protrudes out of the vagina.
Uterine prolapse can occur in women of any age. But it often affects postmenopausal women who’ve had one or more vaginal deliveries.
Mild uterine prolapse usually doesn’t require treatment. But if uterine prolapse makes you uncomfortable or disrupts your normal life, you might benefit from treatment.

- Muscle weakness or relaxation may allow your uterus to sag or come completely out of your body in various stages:
- First degree: The cervix drops into the vagina.
- Second degree: The cervix drops to the level just inside the opening of the vagina.
- Third degree: The cervix is outside the vagina.
- Fourth degree: The entire uterus is outside the vagina. This condition is also called procidentia. This is caused by weakness in all of the supporting muscles.
- Other conditions are usually associated with prolapsed uterus. They weaken the muscles that hold the uterus in place:
- Cystocele: A herniation (or bulging) of the upper front vaginal wall where a part of the bladder bulges into the vagina. It’s also called a prolapsed bladder. This may lead to urinary frequency, urgency, retention, and incontinence (loss of urine).
- Enterocele: The herniation of the upper rear vaginal wall where a small bowel portion bulges into the vagina. Standing leads to a pulling sensation and backache that is relieved when you lie down.
- Rectocele: The herniation of the lower rear vaginal wall where the rectum bulges into the vagina. This makes bowel movements difficult, to the point that you may need to push on the inside of your vagina to empty your bowel.
Causes
Uterine prolapse results from the weakening of pelvic muscles and supportive tissues. Causes of weakened pelvic muscles and tissues include:
- Pregnancy
- Difficult labor and delivery or trauma during childbirth
- Delivery of a large baby
- Being overweight or obese
- Lower estrogen level after menopause
- Chronic constipation or straining with bowel movements
- Chronic cough or bronchitis
- Repeated heavy lifting
Symptoms
Women who have a minor uterine prolapse may not have any symptoms. Moderate to severe prolapse may cause symptoms, such as:
- the feeling that you’re sitting on a ball
- vaginal bleeding
- increased discharge
- problems with sexual intercourse
- the uterus or cervix protruding out of the vagina
- a pulling or heavy feeling in the pelvis
- constipation or difficulty passing stool
- recurring bladder infections or difficulty emptying your bladder
If you develop these symptoms, you should see your doctor and get treatment right away. Without proper attention, the condition can impair your bowel, bladder, and sexual function.
Mild uterine prolapse generally doesn’t cause signs or symptoms. Signs and symptoms of moderate to severe uterine prolapse include:
- Sensation of heaviness or pulling in your pelvis
- Tissue protruding from your vagina
- Urinary problems, such as urine leakage (incontinence) or urine retention
- Trouble having a bowel movement
- Feeling as if you’re sitting on a small ball or as if something is falling out of your vagina
- Sexual concerns, such as a sensation of looseness in the tone of your vaginal tissue
Often, symptoms are less bothersome in the morning and worsen as the day goes on.
When to see a doctor
See your doctor to discuss your options if signs and symptoms of uterine prolapse become bothersome and disrupt your normal activities

Risk factors
Factors that can increase your risk of uterine prolapse include:
- One or more pregnancies and vaginal births
- Giving birth to a large baby
- Increasing age
- Obesity
- Prior pelvic surgery
- Chronic constipation or frequent straining during bowel movements
- Family history of weakness in connective tissue
- Being Hispanic or white
Complications
Uterine prolapse is often associated with prolapse of other pelvic organs. You might experience:
- Anterior prolapse (cystocele). Weakness of connective tissue separating the bladder and vagina may cause the bladder to bulge into the vagina. Anterior prolapse is also called prolapsed bladder.
- Posterior vaginal prolapse (rectocele). Weakness of connective tissue separating the rectum and vagina may cause the rectum to bulge into the vagina. You might have difficulty having bowel movements.
Severe uterine prolapse can displace part of the vaginal lining, causing it to protrude outside the body. Vaginal tissue that rubs against clothing can lead to vaginal sores (ulcers.) Rarely, the sores can become infected
diagnosis
Your doctor can diagnose uterine prolapse by evaluating your symptoms and performing a pelvic exam. During this exam, your doctor will insert a device called a speculum that allows them to see inside of the vagina and examine the vaginal canal and uterus. You may be lying down, or your doctor may ask you to stand during this exam.
Your doctor may ask you to bear down as if you’re having a bowel movement to determine the degree of prolapse.
Your health care provider can diagnose uterine prolapse with a medical history and physical examination of the pelvis.
- The doctor may need to examine you in standing position and while you are lying down and ask you to cough or strain to increase the pressure in your abdomen.
- Specific conditions, such as ureteral obstruction due to complete prolapse, may need an intravenous pyelogram (IVP) or renal sonography. Dye is injected into your vein, and a series of X-rays are taken to view its progress through your bladder.
- Ultrasound may be used to rule out other pelvic problems. In this test, a wand is passed over your abdomen or inserted into your vagina to create images with sound waves.
- Pelvic magnetic resonance imaging (MRI) is sometimes done if you have more than one prolapsed organ or to help plan surgery.
Prevention
To reduce your risk of uterine prolapse, try to:
- Perform Kegel exercises regularly. These exercises can strengthen your pelvic floor muscles — especially important after you have a baby.
- Treat and prevent constipation. Drink plenty of fluids and eat high-fiber foods, such as fruits, vegetables, beans and whole-grain cereals.
- Avoid heavy lifting and lift correctly. When lifting, use your legs instead of your waist or back.
- Control coughing. Get treatment for a chronic cough or bronchitis, and don’t smoke.
- Avoid weight gain. Talk with your doctor to determine your ideal weight and get advice on weight-loss strategies, if you need them.

treatment
Treatment isn’t always necessary for this condition. If the prolapse is severe, talk with your doctor about which treatment option is appropriate for you.
Nonsurgical treatments include:
- losing weight to take stress off pelvic structures
- avoiding heavy lifting
- doing Kegel exercises, which are pelvic floor exercises that help strengthen the vaginal muscles
- wearing a pessary, which is a device inserted into the vagina that fits under the cervix and helps push up and stabilize the uterus and cervix
The use of vaginal estrogen has been well-studied and shows improvement in vaginal tissue regeneration and strength. While using vaginal estrogen to help augment other treatment options may be helpful, on its own it doesn’t reverse the presence of a prolapse.
Surgical treatments include uterine suspension or hysterectomy. During uterine suspension, your surgeon places the uterus back into its original position by reattaching pelvic ligaments or using surgical materials. During a hysterectomy, your surgeon removes the uterus from the body through the abdomen or the vagina.
Surgery is often effective, but it’s not recommended for women who plan on having children. Pregnancy and childbirth can put an immense strain on pelvic muscles, which can undo surgical repairs of the uterus.
Treatment of uterine prolapse is largely dependent on the extent to which a patient is experiencing symptoms. Treatments include surgical and non-surgical options, the choice of which will depend on general health, the severity of the condition and plans for a future pregnancy.
Proper diagnosis and management of uterine prolapse can majorly impact a patient’s quality of life and can have long-term physical and mental health effects. Healthcare practitioners should thoroughly counsel patients with uterine prolapse so they can make informed decisions and choose the treatment that is right for them.
Options include:
- Pelvic floor exercises
- Vaginal pessary
- Vaginal surgery.
- Pelvic floor muscle training:
- Typically taught to patients in association with a physiotherapist. They have been shown to result in subjective improvement in symptoms by patients as well as objective improvement in the The Pelvic Organ Prolapse Quantification (POP-Q) system score by examiners.
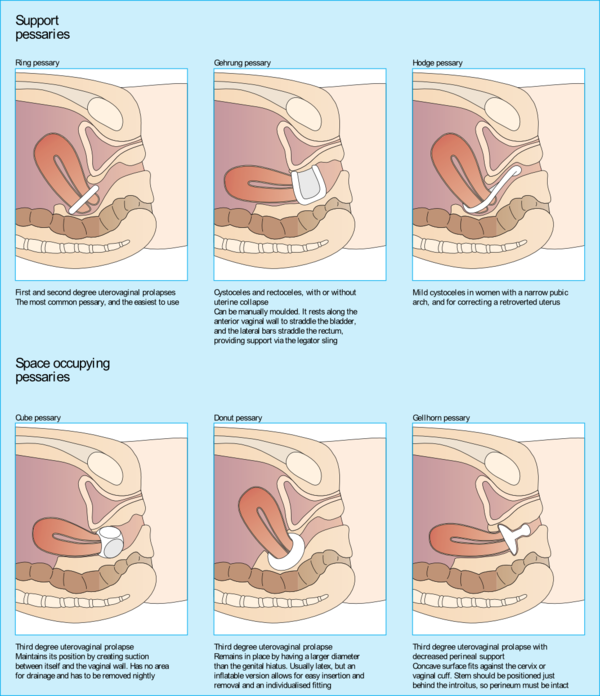
2. Vaginal pessaries:
- Objects often made of silicone that are inserted into the vagina to provide support for the prolapsed pelvic organs.
- Vaginal pessaries can be an effective way of reducing the symptoms of a prolapse, but they will not be appropriate for everyone. Together with pelvic floor exercises, they may provide a non-surgical solution to manage a uterine prolapse.
- Vaginal pessaries provide a solution in 84% of cases of advanced pelvic organ prolapse with mild adverse events in 31% of cases.
- Patients must be fitted for a pessary and commonly try several pessaries before finding the appropriate one. The examiner should be able to sweep a single finger between the pessary and vaginal walls. The patient should be able to walk, bend, and urinate comfortably without shifting the pessary. Complications of pessary placement include vaginal irritation/ulceration, discharge, pain, bleeding, and odor.
- Regular reassessments of pessary fit should be performed to ensure that the pessary is not rubbing against the walls of the vagina, as this can lead to irritation of the vaginal mucosa and predispose patients to infection. Patients with dementia or poor follow up are not good candidates for pessary placement as they require frequent cleaning and regular reassessment of position to prevent complications.
Surgical management
- Decision should be made after a detailed discussion with the patient regarding the desire for future vaginal intercourse, effects on body image, cultural views, alternative treatments, and potential complications.
- In moderate to severe cases, the prolapse may have to be surgically repaired. In laparoscopic surgery, instruments are inserted through the navel. The uterus is pulled back into its correct position and reattached to its supporting ligaments. The operation can also be performed with an abdominal incision.
- Surgery may fail and the prolapse can recur if the original cause of the prolapse, such as obesity, coughing or straining, is not addressed.
Physiotherapy
Physical therapists play a major role in the nonsurgical management of Uterine prolapse. Along with pessary support, pelvic-floor muscle training (PFMT) is cited in highly credible reviews as a main nonsurgical option for women with Uterine prolapse.
For all the information re retraining these muscles see the physiotherapy section of Pelvic Floor Dysfunction and Kegel’s Exercises
In a study by Panman et al in 2016, examining the two-year effects of pelvic floor muscle retraining, it was demonstrated that in women aged 55 and greater with symptomatic mild pelvic organ prolapse, pelvic floor muscle retraining results in a significant decrease in pelvic floor symptoms when compared to watchful waiting (note: statistically significant but below the minimal clinically important difference). Additionally, it was found that pelvic floor muscle retraining was more effective in women who experienced increased pelvic floor symptom distress at baseline. Conversely, the same study found no difference in sexual functioning, quality of life, function of the pelvic floor muscles or degree of prolapse.
A randomised control trial compared the effect of intravaginal vibratory stimulation (IVVS) with intravaginal electrical stimulation (IVES) in women with pelvic floor dysfunctions, unable to voluntarily contract the pelvic floor muscles. The results showed improvement with both techniques, with IVVS superior to IVES in improving pelvic floor muscle strength.
Pelvic floor muscle retraining included: (Kegel exercises diagram in illustration)
- Explanation and description of the pelvic floor
- Instruction regarding how to contract and relax pelvic floor muscles
- If unable to perform this task, use feedback through digital palpation
- If insufficient control demonstrated, use myofeedback or electrical stimulation
- General exercise program provided, subsequently modified for individual needs
- Taught correct technique for contracting pelvic floor muscles before and during increases in abdominal pressure
- Received information about washroom habits and lifestyle
- If pelvic floor muscles were overactive, focus was on relaxation rather than contraction
- Face-to-face contact with physiotherapist as well as encouragement to maintain practice at home 3-5 times per week, 2-3 times per day
Thanks for sharinig a valuable information for more info log on to: https://www.drnaseem.com.au/
LikeLike
Howdy! I could have sworn I’ve been to this web site before but after browsing through many of the articles I realized it’s new to me. Regardless, I’m certainly delighted I discovered it and I’ll be bookmarking it and checking back often!
LikeLike
Howdy, There’s no doubt that your web site might be having internet browser compatibility issues. Whenever I take a look at your site in Safari, it looks fine but when opening in Internet Explorer, it’s got some overlapping issues. I merely wanted to give you a quick heads up! Besides that, excellent site!
LikeLike
REQUEST AN APPOINTMENT OR BOOK A CONSULANT – Sargam.dange.18@gmail.com
LikeLike
Greetings! Very helpful advice in this particular article! It is the little changes which will make the most significant changes. Thanks a lot for sharing!
LikeLike
REQUEST AN APPOINTMENT OR BOOK A CONSULANT – Sargam.dange.18@gmail.com
LikeLike
We’re a bunch of volunteers and starting a new scheme in our community. Your web site offered us with helpful info to work on. You have done a formidable activity and our entire neighborhood shall be grateful to you.
LikeLike
REQUEST AN APPOINTMENT OR BOOK A CONSULANT – Sargam.dange.18@gmail.com
LikeLike