REQUEST AN APPOINTMENT OR BOOK A CONSULANT – Sargam.dange.18@gmail.com
The pelvis is a ring of bone at hip level, made up of several separate bones. A pelvic fracture is a break in any one of those bones. Some pelvic fractures involve breaking more than one of the bones, and these are particularly serious as the bones are more likely to slip out of line.
The pelvis is the sturdy ring of bones located at the base of the spine. Fractures of the pelvis are uncommon—accounting for only about 3% of all adult fractures.
Most pelvic fractures are caused by some type of traumatic, high-energy event, such as a car collision. Because the pelvis is in proximity to major blood vessels and organs, pelvic fractures may cause extensive bleeding and other injuries that require urgent treatment.

In some cases, a lower-impact event—such as a minor fall—may be enough to cause a pelvic fracture in an older person who has weaker bones.
Treatment for a pelvic fracture varies depending on the severity of the injury. While lower-energy fractures can often be managed with conservative care, treatment for high-energy pelvic fractures usually involves surgery to reconstruct the pelvis and restore stability so that patients can resume their daily activities.
types of pelvic fracture
Because the pelvis is a ring of bones, when forceful injury causes a fracture in one part of the structure, there is often a matching fracture at the opposite point in the ring. There are several common patterns, which depend upon the direction and severity of the trauma.
Stable and unstable fractures
Perhaps the most important way of classifying pelvic fractures is into stable or unstable fractures. Most pelvic fractures are stable:
Stable fracture: the broken bones are still properly lined up, so that the ring has kept its shape. Usually only one bone is affected, with a single fracture.
Common fracture patterns include: breaks across the top of one ilium, cracks to the pubic ramus on one side, or cracks in the sacrum. In each of these cases the other bones are intact and will keep the bony ring of the pelvis together. Pelvic avulsion fractures (in which a fragment of bone is broken off by the pull of a muscle) and pelvic stress fractures (hairline cracks which do not extend all the way across the bone) are also types of stable pelvic fractures.
Unstable fracture: this usually occurs when there are two or more breaks in the pelvic ring and the ends of the broken bones move apart. This type of fracture is more likely to occur after high-impact injury and there may, therefore, be other associated injuries.
These injuries involve much more bleeding than stable fractures, as the separation of the broken bones allows them to bleed much more freely. They may also involve direct damage to the internal organs.
There are some typical patterns of unstable fractures. These include ‘open book’ fractures, when the pelvis is broken at the front and the back by severe force from the front, and lateral (or sideways) force fractures which often fracture the pubic rami and the sacroiliac joints, sometimes also involving the hip socket.
Open and closed fractures
Pelvic fractures, whether stable or unstable, can also be divided into ‘open’ fractures, in which injuries to the skin mean that the broken bones are visible, or ‘closed’ fractures, in which the skin is not broken. Open fractures are more serious because infection can easily reach the wound, which may already be contaminated from the injury.
Description
Because the pelvis is a ring-like structure, a fracture in one part of the structure is often accompanied by a fracture or damage to ligaments at another point in the structure. Doctors have identified several common pelvic fracture patterns. The specific pattern of the fracture depends upon the direction in which it was broken and the amount of force that caused the injury.
In addition to being described by the specific fracture pattern, pelvic fractures are often described as “stable” or “unstable,” based on how much damage has occurred to the structural integrity of the pelvic ring.
Stable fracture. In this type of fracture, there is often only one break in the pelvic ring and the broken ends of the bones line up adequately. Low-energy fractures are often stable fractures. Stable pelvic fracture patterns include:
Types of stable pelvic fractures: (Left) Iliac wing fracture. (Right) Sacrum fracture.
Superior and inferior pubic ramus fracture
Unstable fracture. In this type of fracture, there are usually two or more breaks in the pelvic ring and the ends of the broken bones do not line up correctly (displacement). This type of fracture is more likely to occur due to a high-energy event. Unstable pelvic fracture patterns include:
Types of unstable pelvic fractures: (Left) Anterior-posterior compression fracture. (Right) Lateral compression fracture. In this fracture, the pelvis is pushed inward.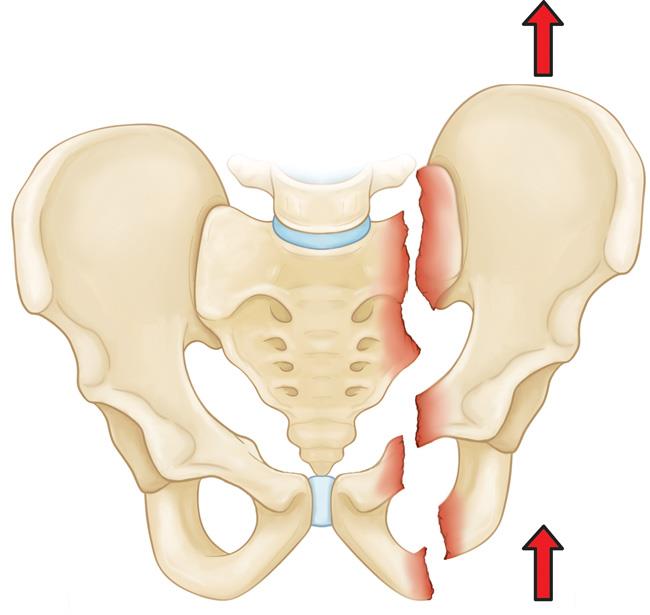
Vertical shear fracture. In this fracture, one half of the pelvis shifts upward.
Both stable and unstable pelvic fractures can also be divided into “open” fractures, in which the bone fragments stick out through the skin, or “closed” fractures, in which the skin is not broken. Open fractures are particularly serious because, once the skin is broken, infection in both the wound and the bone can occur. Immediate treatment is required to prevent infection.
Cause
Major pelvic fractures are caused by major trauma such as road traffic accidents, crush injuries (for example, being run over by a car or rolled on by a horse) and falls from height. Pelvic fractures caused by high-force or high-speed injuries are often unstable and they need urgent hospital treatment.
Less severe fractures which involve undisplaced fractures can occur after falls or trips, particularly if the bones are ‘thin’ (osteoporosis). For this reason painful but stable fractures are more common in elderly people who tend to have ‘thinner’ bones, and who are sometimes prone to falls.
REQUEST AN APPOINTMENT OR BOOK A CONSULANT – Sargam.dange.18@gmail.com
What causes pelvic avulsion fractures?
A pelvic avulsion fracture occurs when the tendon of a muscle comes away from the bone, taking a small chip of bone with it. This most commonly occurs at bottom of the ischium where the big hamstring muscles are attached, or on the front of the ilium where one of the large quadriceps muscles attaches.
These types of fractures typically occur during sports that involve speed and sudden stops, particularly in young people who are still growing. Examples are hurdling, sprinting, long-jumping, and soccer (particularly miskicks that hit the ground). A pelvic avulsion fracture may also be caused by a car accident.
What causes pelvic stress fractures?
Pelvic stress fractures are caused by repeated stresses to the bone, usually due to sport. They usually affect the pubic bone and cause exercise-related pain which gets gradually worse, but they do not usually prevent exercise. Sports involving repeated impact, such as running or jumping, carry the highest risk. Stress fractures often occur in those who suddenly increase their training distance or activity level, including sedentary people who suddenly start to exercise. They are uncommon in the pelvis, although more common in women and those with ‘thinning’ of the bones (osteoporosis).
Who has pelvic fractures?
Significant pelvic fractures can occur in anyone who experiences a major trauma. Less severe, stable fractures are most commonly seen in elderly people, particularly those with ‘thinner’ bones (osteoporosis). Avulsion fractures are particularly common in sporty teenagers. Stress fractures are typically seen in runners, although they more commonly affect other sites than the pelvis.
High-Energy Trauma
A pelvic fracture may result from a high-energy force, such as that generated during a:
- Car or motorcycle collision
- Crush accident
- Fall from a significant height (such as a ladder)
Depending on the direction and magnitude of the force, these injuries can be life-threatening and require surgical treatment.
Bone Insufficiency
A pelvic fracture may also occur due to weak or insufficient bone. This is most common in older people whose bones have become weakened by osteoporosis. In these patients, a fracture may occur even during a fall from standing or a routine activity such as getting out of the bathtub or descending stairs. These injuries are typically stable fractures that do not damage the structural integrity of the pelvic ring, but may fracture an individual bone.
Other Causes
Less commonly, a fracture may occur when a piece of the ischium bone tears away from the site where the hamstring muscles attach to the bone. This type of fracture is called an avulsion fracture and it is most common in young athletes who are still growing. An avulsion fracture does not usually make the pelvis unstable or injure internal organs.
Symptoms
A fractured pelvis is almost always painful. This pain is aggravated by moving the hip or attempting to walk. Often, the patient will try to keep his or her hip or knee bent in a specific position to avoid aggravating the pain. Some patients may experience swelling or bruising in the hip area.
What causes pelvic avulsion fractures?
A pelvic avulsion fracture occurs when the tendon of a muscle comes away from the bone, taking a small chip of bone with it. This most commonly occurs at bottom of the ischium where the big hamstring muscles are attached, or on the front of the ilium where one of the large quadriceps muscles attaches.
These types of fractures typically occur during sports that involve speed and sudden stops, particularly in young people who are still growing. Examples are hurdling, sprinting, long-jumping, and soccer (particularly miskicks that hit the ground). A pelvic avulsion fracture may also be caused by a car accident.
What causes pelvic stress fractures?
Pelvic stress fractures are caused by repeated stresses to the bone, usually due to sport. They usually affect the pubic bone and cause exercise-related pain which gets gradually worse, but they do not usually prevent exercise. Sports involving repeated impact, such as running or jumping, carry the highest risk. Stress fractures often occur in those who suddenly increase their training distance or activity level, including sedentary people who suddenly start to exercise. They are uncommon in the pelvis, although more common in women and those with ‘thinning’ of the bones (osteoporosis).
Who has pelvic fractures?
Significant pelvic fractures can occur in anyone who experiences a major trauma. Less severe, stable fractures are most commonly seen in elderly people, particularly those with ‘thinner’ bones (osteoporosis). Avulsion fractures are particularly common in sporty teenagers. Stress fractures are typically seen in runners, although they more commonly affect other sites than the pelvis.
What are the symptoms of stable pelvic fractures?
A stable pelvic fracture is almost always painful. Pain in the hip or groin is usual and is made worse by moving the hip or trying to walk – although walking may still be possible. Some patients find if they try to keep one hip or knee bent this can ease the pain.
Other symptoms will vary with the severity. They may include:
- Pain and tenderness in the groin, hip, lower back, buttock or pelvis.
- Bruising and swelling over the pelvic bones.
- Numbness or tingling in the genital area or in the upper thighs.
- Pain which may also be present on sitting and when having a bowel movement.
There may also be visible signs of bleeding. Bleeding can track out to the skin in several places, some of which are more likely to be visible than others. They include:
- Bruising over the pelvic bones themselves.
- Bruising or a tender lump in the groin or on the perineum.
- Bruising in the small of the back.
- Vaginal bleeding in women, and bruising to the scrotum in men.
- Blood in the urine or coming from the back passage.
Note: after significant trauma, such as a road accident, serious pelvic fracture is quite likely, even in patients who are initially walking around. It is really important if assisting at the scene of an accident, therefore, to keep survivors still and warm until emergency services arrive. This will reduce risk of dangerous bleeding and may save lives.
What are the symptoms of unstable pelvic fractures?
Major and unstable pelvic fractures are likely to cause severe pain and shock. Pain may be in the pelvis, groin, back, tummy (abdomen), or down the legs.
The pelvic bones are large and have a rich blood supply, so when broken they will bleed heavily and the bleeding will not stop quickly. Whilst the blood may not be visible, because it is on the inside of your tummy, this level of blood loss will cause a sudden drop in your blood pressure. Affected people will be pale, clammy and seriously unwell, perhaps even unconscious.
It is sometimes possible to move around and attempt to walk immediately after a major unstable pelvic fracture – particularly after road accidents. This is because shock can initially prevent you from feeling pain.
What are the symptoms of pelvic avulsion fractures?
Pelvic avulsion fractures are mainly seen in young, active sportspeople who are still growing. Symptoms are usually of sudden pain during a sudden powerful movement. The pain is often in the bottom, in the crease of the buttock, or at the bony part on the front of the hip. Afterwards the athlete will feel weakness and pain when doing the movements which use the affected tendon and muscle. Bruising and swelling are likely.
REQUEST AN APPOINTMENT OR BOOK A CONSULANT – Sargam.dange.18@gmail.com
What are the symptoms of pelvic stress fractures?
Stress fractures – where there is a fine crack in the bone which does not extend all the way through – are one of the mildest sorts of stable fracture. Stress fractures of the pelvis are easy to miss as the pain may be quite hard to locate. Symptoms typically consist of a dull pain that is difficult to localise at first. This may get better as exercise continues but be worse afterwards

Doctor Examination
Emergency Stabilization
Patients with high-energy fractures will almost always go or be brought to an urgent care center or emergency room for initial treatment due to the severity of their symptoms.
These patients may also have additional injuries to the head, chest, abdomen, or legs. If their injuries cause significant blood loss, it could lead to shock—a life-threatening condition that can result in organ failure.
The care of patients with high-energy pelvic fractures requires a multidisciplinary approach with input from a number of medical specialists. In some cases, doctors must address airway, breathing, and circulatory problems before treating the fracture and other injuries.
Physical Examination
Your doctor will carefully examine your pelvis, hips, and legs. He or she will also check for nerve injury by assessing whether you can move your ankles and toes and feel sensation on the bottom of your feet.
Your doctor will also carefully examine the rest of your body to determine if you have sustained any other injuries.
Imaging Studies
X-rays. These studies provide images of dense structures, such as bones. All pelvic fractures require x-rays—usually from a number of different angles—to help the doctor determine how displaced place the bones are.
Computed tomography (CT) scans. Because of the complexity of this type of injury, a CT scan is commonly ordered for pelvic fractures. A CT scan will provide a more detailed, cross-sectional image of the pelvis. Your doctor will use this information to better determine the specific pattern and extent of your injury, look for associated injuries, and aid in preoperative planning.
Magnetic resonance imaging (MRI) scans: In rare cases, your doctor may order an MRI scan to discover a fracture that cannot be seen on x-ray or CT scan.
in the case of major injuries, such as road traffic accidents, where pelvic fracture is likely and must be excluded, X-rays will be performed urgently to assess the state of the pelvic bones. A pelvic fracture is also suspected if you have had a lesser injury but there is pelvic bone tenderness, difficulty walking or any loss of sensation in the lower part of the body.
X-ray will show most pelvic bone injuries, although it will not show details of injuries to organs inside the pelvis. X-rays provide images of bones and in the case of the pelvis, they are usually taken from a number of different angles, so that doctors can check whether (and how much) the bones are out of line.
A computerised tomography (CT) scan involves multiple X-rays in ‘slices’ down through the pelvis in order to build up a three-dimensional image of the injuries. This will be done in complicated cases to get a better picture of the fractures and to look for associated injuries.
A magnetic resonance image (MRI) scan is an alternative to CT and may give a clearer picture of damage. This is not usually necessary, except in the case of stress fractures, which can show up well on MRI scanning but which commonly are not visible on X-ray or CT.
Ultrasound scans and contrast studies (where a radioactive dye is injected to create pictures to enable doctors to check on internal organs and structures) may be needed to assess internal organs.
Radioisotope bone scans are sometimes used to look for stress fractures, particularly in patients who cannot have an MRI scan (for example, if they have a pacemaker).
If your fracture happened unusually easily, and your doctor thinks there is a possibility that you have underlying ‘thinning’ of the bones (osteoporosis), you may be offered a bone scan to check your bone density. This scan is called dual-energy X-ray absorptiometry (DXA – formerly DEXA).
Other investigations may include blood tests to assess the degree of blood loss and the function of the liver and kidneys, and testing of the urine to look for damage to the bladder.
First aid in pelvic fracture
Until help arrives a person with a suspected pelvic fracture should be covered with a blanket or jacket and should not be moved by non-trained personnel, especially if there is severe pain.
If you are at a serious road accident and a person is walking around, get them to sit still. Ask if there is any pain anywhere, particularly in their chest, tummy (abdomen) or hips. If there is pain anywhere near the pelvis they could have a major pelvic fracture, and you should assume they are seriously injured and keep them still and warm until emergency services arrive. It is well known that sometimes people walk around with severe pelvic fractures immediately after road accidents, as shock can prevent them from initially feeling much pain.
Treatment
Treatment is based on a number of factors, including:
- The specific pattern of the fracture
- How much the bones are displaced
- Your overall condition and associated injuries
Nonsurgical Treatment
Your doctor may recommend nonsurgical treatment for stable fractures in which the bones are nondisplaced or minimally displaced.
Nonsurgical treatments may include:
Walking aids. To avoid bearing weight on your leg, your doctor may recommend that you use crutches or a walker for up to three months—or until your bones are fully healed. If you have injuries above both legs, you may need to use a wheelchair for a period of time so that you can avoid bearing weight on either leg.
Medications. Your doctor may prescribe medication to relieve pain, as well as an anti-coagulant, or blood thinner, to reduce the risk of blood clots forming in the veins of your legs and pelvis.
Surgical Treatment
Patients with unstable pelvic fractures may require one or more surgical procedures.
External fixation. Your doctor may use external fixation to stabilize your pelvic area. In this operation, metal pins or screws are inserted into the bones through small incisions into the skin and muscle. The pins and screws project out of the skin on both sides of the pelvis where they are attached to carbon fiber bars outside the skin. The external fixator acts as a stabilizing frame to hold the broken bones in proper position.
In some cases, an external fixator is used to stabilize the bones until healing is complete. In patients who are unable to tolerate a lengthy, more complicated procedure, an external fixator may be used as a temporary treatment until another procedure can be performed.
Skeletal traction. Skeletal traction is a pulley system of weights and counterweights that helps realign the pieces of bone. Skeletal traction is often used immediately after an injury and removed after surgery. Occasionally, acetabular fractures can be treated with skeletal traction alone. This is rare, however, and will be a decision made jointly with input from your doctor.
During skeletal traction, metal pins are implanted in the thighbone or shinbone to help position the leg. Weights attached to the pins gently pull on the leg, keeping the broken bone fragments in as normal a position as possible. For many patients, skeletal traction also provides some pain relief.
Open reduction and internal fixation. During this operation, the displaced bone fragments are first repositioned (reduced) into their normal alignment. They are then held together with screws or metal plates attached to the outer surface of the bone.
External pelvic fixation
This involves long screws inserted into the bones from the sides and a large external frame. It is done in the operating theatre, under anaesthetic. It helps prevent further blood loss by holding the bones together. The metal pins or screws are inserted into the bones through small incisions into the skin and muscle. They project out of the skin on both sides of the pelvis where they are attached to carbon fibre bars. The external fixator acts as a stabilising frame to hold the bones in proper position.
Traction
This involves a pulley system of external pins in the bones, with weights and counterweights. It helps line up the pieces of bone. Skeletal traction is sometimes used as a temporary treatment, and it often provides some pain relief. Occasionally, pelvic fractures are treated with skeletal traction alone but this is unusual.
Internal pelvic fixation
A few patients require internal fixation to keep the bones in place. This is open surgery, performed under anaesthetic. The bone fragments are repositioned, then held together with screws or metal plates which are left permanently in place. Getting the pelvis fixed and stable is very important both for pain control and for the long-term results of your treatment. It is more likely to be necessary if there are multiple fractures.
Management of pain
Pain is managed using painkillers and by stabilising an unstable pelvis. Strong painkillers and local anaesthetics may initially be needed. You may at first have an epidural anaesthetic to help manage the initial pain.
Blood clots
Doctors usually prescribe ‘blood thinners’ (anticoagulants) to reduce the risk of blood clots forming in the veins of your legs and pelvis. Pelvic fractures are known to increase the risk of blood clots.
Bed rest
Initial treatment is with pain relief and bed rest, followed by mobilisation. Doctors will want to get you moving as soon as possible, as this is better for your long-term recovery, and also reduces the risk of blood clots forming (deep vein thrombosis). However, you are likely to need to use crutches or a walker for around three months, or until your bones are fully healed. If you have injuries above both legs, you may need to use a wheelchair for a period of time so that you can avoid putting any weight on either leg.
Physiotherapy
You will be seen regularly by physiotherapists who will try to help you keep muscle strength and joint mobility whilst you are not able to weight bear.
Once you start to weight bear, physiotherapy will still be needed to strengthen your muscles and help you regain your balance, as you may find this is much less good when you first start walking again.
How are stable pelvic fractures treated?
With a stable fracture, the most common treatment is bed rest and prescribed painkillers.
Surgical treatment is not usually needed for stable fractures. Crutches and walking aids are likely to be used as part of your recovery, and physiotherapy will be an essential part of your treatment.
How are pelvic avulsion fractures treated?
Treatment of pelvic avulsion fractures is with rest. These fractures usually heal by themselves over 4-6 weeks. Initially, applying ice can help pain and inflammation.
Occasionally, surgery is needed to re-attach the bone and tendon to the pelvis; however, this is mainly reserved for unusually large avulsion fractures.
Following the rest period, a gradual rehabilitation programme can be commenced which aims to regain full strength and movement at the hip.
How are pelvic stress fractures treated?
Pelvic stress fractures can cause lingering, worsening pain and may become full-thickness fractures, so rest from the activity which caused them is very important. A gradual reintroduction to running can begin after a few weeks, once the athlete is pain-free.
Some specialists now suggest treatment with an infusion of pamidronate, a drug more commonly used to treat ‘thinning’ of the bones (osteoporosis). This treatment appears to be fairly effective in speeding the healing of stress fractures, even in patients without osteoporosis.
Complications
There are risks associated with any surgical procedure. Before your surgery, your doctor will discuss each of these risks with you and will take specific measures to help avoid potential complications.
Possible complications include:
- Wound healing problems, including infection
- Damage to nerves or blood vessels
- Blood clots
- Pulmonary embolism—a blood clot in the lungs
REQUEST AN APPOINTMENT OR BOOK A CONSULANT – Sargam.dange.18@gmail.com